Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare syndrome characterized by life-threatening inflammation. In adults, roughly 50% of HLH manifests in association with an underlying malignancy (most commonly lymphoma), and the remaining cases are due to infection, autoimmune disease, late presentations of genetically-driven HLH, and sometimes multifactorial or idiopathic causes. Although the majority of prospective data for HLH are derived from children, survival outcomes for non-malignant causes of adult HLH (nmHLH) are thought to rival pediatric HLH; however, outcomes for malignancy-associated HLH (mHLH) appear to be substantially worse (~10-30% 5-year overall survival) in the literature. As diagnostic and prognostic models for HLH outcomes have primarily been constructed using pediatric data, attempts have been made to develop diagnostic indices applicable to adult HLH (particularly mHLH). Here, we summarize the clinical and laboratory characteristics of mHLH and nmHLH in a retrospective observational study, and evaluate the role for common diagnostic tools for adult HLH.
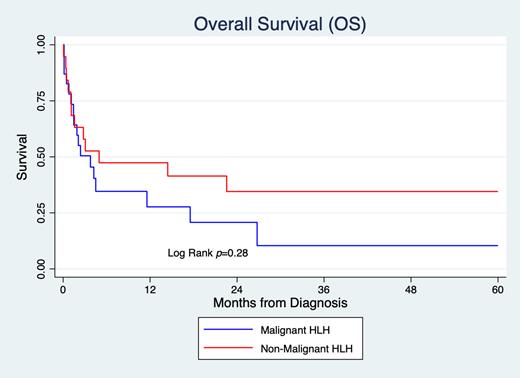
Methods: Patients >18 years old, fulfilling at least five of the HLH-2004 diagnostic criteria with at least 3 months of follow-up (among survivors) were enrolled. All included patients received definitive HLH therapy, including cancer-directed therapy when appropriate, but those receiving only systemic steroids were excluded. Treatment-related HLH, such as HLH occurring with immune effector cell therapy or hematopoietic cell transplantation, was excluded. Clinical and laboratory parameters reflect the most recent values on or prior to diagnosis and treatment initiation. Differences between mHLH and nmHLH were assessed with two-tailed t-test or Wilcoxon test. Survival outcomes are estimated by Kaplan-Meier. Multivariate analysis was performed using Cox proportional hazards and compared using logrank test.
Results: 42 adults were diagnosed with HLH requiring HLH-specific therapy (23 mHLH, 19 nmHLH) between 3/2016 and 3/2023 with a median age of 50 (range 21-75). Of the mHLH cases, 44% were due to T/NK cell lymphomas; 52% were B cell lymphomas including 26% Hodgkin. Of the nmHLH cases, most were due to infection (47%); while others were deemed to be idiopathic (26%) or genetic (16%). All patients with mHLH had fever (v 84% in nmHLH); 91% met cytopenia criteria (v 68%), and absolute neutrophil count (ANC), hemoglobin (Hgb), and platelet count (plt) were all statistically lower than in nmHLH (mean ANC 3.2 v 11.3; Hgb 7.8 v 8.5; plt 43 v 88; p<0.05). Mean soluble interleukin-2 (sIL2) level was significantly higher in mHLH (39,579 pg/mL v 18,484) after adjusting for a single outlier. All other HLH-2004 diagnostic parameters were not statistically different between mHLH and nmHLH, including ferritin and sIL2/ferritin index. All mHLH patients had an underlying lymphoma and met the optimized HLH inflammatory (OHI) index except a single patient with leukemia; 4 patients with nmHLH did not meet the OHI index. In 79% of patients, the HLH94 regimen was incorporated in the induction regimen; the remaining utilized chemotherapy or antibiotics, with and without adjunctive steroids. 4 cases proceeded to allogeneic transplantation. Relapse rates were high, with median relapse-free survival (RFS) being 37 days (23 v 47 days for mHLH and nmHLH, respectively); median overall survival (OS) was 96 days (86 v 149 days). RFS/OS was not statistically different between mHLH and nmHLH. Age was a significant predictor of OS but not RFS; no other diagnostic parameter was predictive, including degree of ferritin or sIL2 elevation. 13 patients were alive at the time of last follow-up (6 mHLH, 7 nmHLH).
Conclusions: In this single center retrospective study, both mHLH and nmHLH requiring HLH-directed therapy demonstrated poor survival outcomes in adults. The degree of cytopenias and sIL2 elevation were more significant in mHLH in comparison with nmHLH. The OHI index identified all cases of lymphoma-associated HLH but neither ferritin nor sIL2 levels were predictive of survival. These data emphasize the need for therapeutic advances for management of adults with mHLH and nmHLH and continued optimization of diagnostic criteria for adult HLH.
Disclosures
Logan:AbbVie, Amgen, Actinium, BMS, Pfizer, Sanofi, Takeda: Consultancy; Amgen, Autolus Therapeutics, Kadmon, Kite, Pharmacyclics, Talaris: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal